Mpox, a viral disease that gained global attention in 2022, has challenged public health systems worldwide. Originally identified in 1958 and named after its discovery in monkeys, this zoonotic illness has evolved from a tropical disease to a significant public health concern.
With fears that it has been discovered in some places in Africa and Europe, how can you stay safe? What are some of the symptoms this disease presents with? Is there any vaccine for it?
Let’s take a deeper look
What is Mpox (Monkeypox)?
First things first!
Mpox, formerly known as monkeypox, is a viral zoonotic disease caused by the monkeypox virus. Discovered in 1958 in a colony of research monkeys, hence its original name, the first human case was recorded in 1970 in the Democratic Republic of the Congo.
For decades, mpox was primarily confined to central and west Africa, with sporadic cases linked to international travel or imported animals.
The virus exists in two distinct genetic clades: the central African (Congo Basin) clade and the west African clade. The Congo Basin clade has historically caused more severe disease and was thought to be more transmissible.
In 2022, a significant multi-country outbreak of mpox, primarily caused by the west African clade, brought the disease into global focus.
According to WHO Director-General Tedros Adhanom Ghebreyesus:
“The emergence of a new clade of mpox, its rapid spread in eastern DRC, and the reporting of cases in several neighboring countries are very worrying…It is clear that a coordinated international response is needed to stop these outbreaks and save lives.”
This outbreak led to a reevaluation of the disease’s transmission patterns and public health implications, as well as the decision by the World Health Organization to rename the disease from monkeypox to mpox to reduce stigma and discrimination.
Mpox Symptoms
According to a infectious disease specialist at Yale Medicine Marwan Azar, MD:
“The rash traditionally seen with mpox starts in the center of the body, the face, or the head, and then moves outward to the extremities. That is the classic presentation…But with the 2022 worldwide outbreak, it did not always follow this pattern. In many cases, lesions were only seen in the genital area or around the anus. It’s important to recognize that these lesions could be mistaken for sexually transmitted diseases, such as syphilis or herpes, which also have lesions in those areas.”
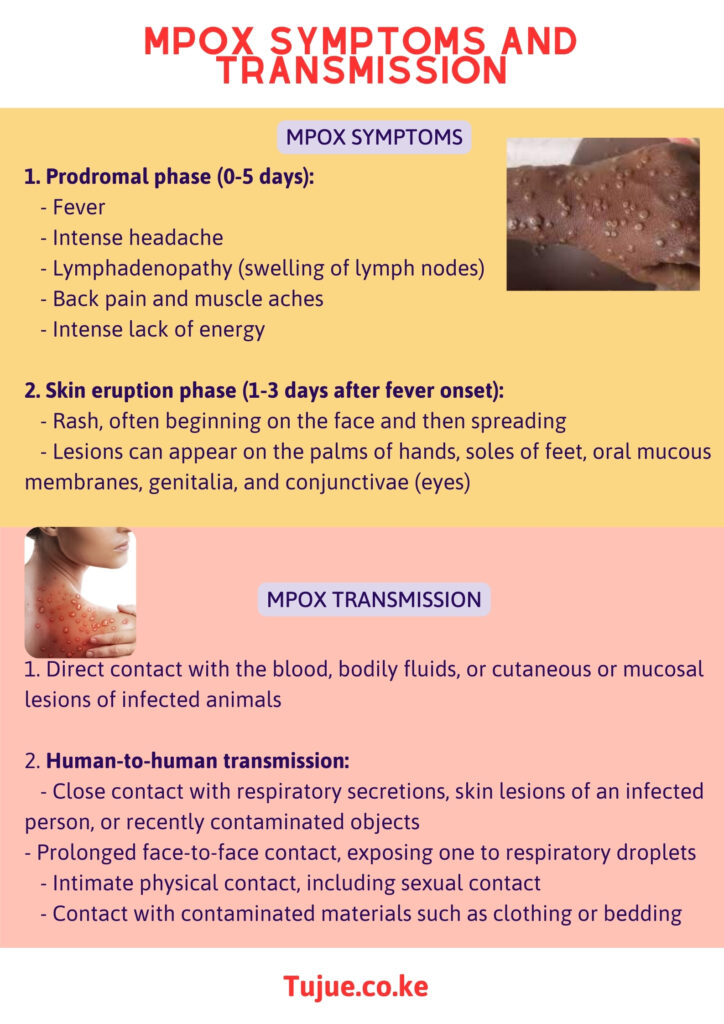
Mpox Symptoms and Transmission Infographic
Mpox symptoms typically appear in two stages:
1. Prodromal phase (0-5 days):
– Fever
– Intense headache
– Lymphadenopathy (swelling of lymph nodes)
– Back pain and muscle aches
– Intense lack of energy
2. Skin eruption phase (1-3 days after fever onset):
– Rash appears, often beginning on the face and then spreading to other parts of the body
– The rash evolves from macules (flat lesions) to papules (raised lesions), vesicles (fluid-filled blisters), pustules, and finally to scabs before falling off
– Lesions can appear on the palms of hands, soles of feet, oral mucous membranes, genitalia, and conjunctivae (eyes)
The number of lesions can vary from a few to several thousand. In severe cases, lesions can coalesce until large sections of skin slough off.
It’s important to note that the 2022 outbreak showed some variations in symptom presentation:
– Some patients reported anorectal pain, rectal bleeding, or proctitis
– Genital and perianal lesions were more common
– Some patients developed lesions before other symptoms
Note: The illness typically lasts for 2-4 weeks. Most cases are mild, but severe cases can occur, particularly in children, pregnant women, or immunocompromised individuals.
How Does Mpox transmit?
According to WHO emergency operations program area manager, Dr. Catherine Smallwood,
“In the African context, we have seen the emergence of this new clade 1b, which is transmitted between humans…We have not detected zoonotic transmission in clade 1b. It seems to be a virus that is circulating exclusively in the human population, and some of the viral changes that virologists have identified show us that it likely transmits more effectively from human to human.”
Mpox transmission occurs through several routes:
1. Animal-to-human transmission:
– Direct contact with the blood, bodily fluids, or cutaneous or mucosal lesions of infected animals
– Handling infected animals, particularly species identified as susceptible to the virus (including rodents and primates)
– Consumption of inadequately cooked meat of infected animals
2. Human-to-human transmission:
– Close contact with respiratory secretions, skin lesions of an infected person, or recently contaminated objects
– Prolonged face-to-face contact, exposing one to respiratory droplets
– Intimate physical contact, including sexual contact
– Contact with contaminated materials such as clothing or bedding
Note: The virus enters the body through broken skin, respiratory tract, or mucous membranes (eyes, nose, or mouth). The incubation period is typically 6 to 13 days but can range from 5 to 21 days.
Is There Mpox Disease Vaccine?
Yes, there are vaccines available that can help prevent mpox infection:
1. JYNNEOS (also known as Imvamune or Imvanex):
– A third-generation vaccine approved for prevention of mpox and smallpox
– Contains a live, non-replicating vaccinia virus
– Administered as a two-dose series, 28 days apart
– Considered safer for immunocompromised individuals
2. ACAM2000:
– Originally developed for smallpox but can be used for mpox under an Expanded Access Investigational New Drug protocol
– Contains live vaccinia virus that can replicate
– Higher risk of side effects compared to JYNNEOS
3. Smallpox vaccines:
– Due to the genetic similarity between the viruses, traditional smallpox vaccines provide some cross-protection against mpox
– Historical data suggests about 85% efficacy in preventing mpox
Vaccination strategies include:
– Pre-exposure prophylaxis for high-risk individuals (e.g., laboratory workers handling orthopoxviruses)
– Post-exposure prophylaxis for close contacts of confirmed cases, ideally within 4 days of exposure
Note: It’s important to note that while vaccination can significantly reduce the risk of infection or severity of the disease, it doesn’t provide 100% protection. Other preventive measures remain crucial.
Mpox Photos and Images
Here’s how Mpox manifests:






Key Takeaway
Mpox has emerged as a significant global health concern, challenging our understanding of infectious diseases and public health responses. From its origins in African wildlife to its current status as a worldwide issue, mpox has demonstrated the interconnectedness of human and animal health, as well as the potential for diseases to evolve and spread in unexpected ways.
The 2022 outbreak served as a wake-up call, highlighting the need for robust surveillance systems, rapid response mechanisms, and international cooperation in managing emerging infectious diseases. It also underscored the importance of clear, accurate communication to combat misinformation and reduce stigma.

